Usability evaluation of the Doctor Saina online consultation
application using the think-aloud method
Faezeh Raje1, Fateme
Moghbeli2 , Zahra Sangsefidi1
, Zahra Sangsefidi1 , Hamed Maktabdar Roshkhar3,
Mohammad Reza Mazaheri Habibi1*
, Hamed Maktabdar Roshkhar3,
Mohammad Reza Mazaheri Habibi1*
1Department of Health Information Technology, Varastegan Institute for Medical Sciences, Mashhad, Iran
2Statistical Data
Analyst- Researcher and Assessment Services, York Region District Board (YRDSB),
Ontario, Canada
3Sadjad University of
Technology, Mashhad, Iran
|
Article Info
|
A B S T R A C T
|
|
Article type:
Research
|
Introduction:
The rapid advancement of technology and economic growth has created both
opportunities and challenges in healthcare accessibility. The unequal
distribution of medical resources, which disproportionately favors
economically developed regions, has led to a decline in the quality and
efficiency of healthcare services in rural and underdeveloped areas,
highlighting the urgent need for innovative solutions. Telemedicine
effectively overcoming geographical barriers and improving access to medical
care. However, usability issues in some of these applications present
significant challenges, potentially compromising service quality and user
experience. This study aimed to evaluate the usability of the Doctor Saina
application, identifying key factors that influence its effectiveness, user
satisfaction, and overall success.
Material
and Methods: In this study, digital health application Doctor Saina
which facilitate online medical consultations, making healthcare services
more accessible, was examined. A laboratory-based usability evaluation was
conducted using a predefined scenario-driven approach and the think-aloud
method with 15 participants. The identified usability issues were categorized
using the Van den Haak classification framework, and their severity was
assessed based on Nielsen’s heuristic evaluation model.
Results:
The average duration of the usability evaluation per
participant was 22.08 minutes. During the evaluation process, 23 issues were
identified by the users, 5 of which had a severity greater than 2. The most
frequent usability issues identified by users were in the Comprehensiveness
category (43.5%). During the evaluation process, 9% of the issues were
resolved by users without facilitator intervention.
Conclusion:
Among the identified usability challenges, layout and comprehensiveness were
reported as the most significant barriers affecting user experience.
Addressing these issues is crucial for enhancing the overall usability,
accessibility, and effectiveness of the Doctor Saina application.
|
|
Article
History:
Received: 2025-04-22
Accepted: 2025-05-10
Published: 2025-05-14
|
|
* Corresponding
author:
Mohammad Reza Mazaheri Habibi
Department of Health Information Technology,
Varastegan Institute for Medical Sciences, Mashhad, Iran
Email:Mazaherim@Varastegan.ac.ir
|
|
Keywords:
Usability Evaluation
Mobile Health Applications
Doctor Saina
Telemedicine
Think-Aloud Method
|
|
Cite this paper as:
Raje F, Moghbeli F, Sangsefidi
Z, Maktabdar Roshkhar H, Mazaheri Habibi MR. Usability evaluation of the
Doctor Saina online consultation application using the think-aloud method. Adv
Med Inform. 2025; 1: 5.
|
Introduction
With the advancement of socioeconomic conditions and the
development of science and technology, healthcare and medical treatment have
significantly improved. However, due to disparities in economic development
between regions and urban-rural areas, the distribution of medical resources
has been skewed toward economically developed regions [1–3].
This unequal distribution of medical resources has led to
inadequate medical conditions and a decline in the quality and efficiency of
healthcare services in various areas. Consequently, access to medical care
remains a significant challenge for many people. Addressing the issue of
medical resource allocation and ensuring the effective sharing of these
resources is crucial for improving healthcare services and enhancing the
quality of medical care, particularly in underserved regions [4].
Telemedicine has been defined by the World Health
Organization (WHO) as “the delivery of healthcare services by healthcare
professionals using information and communication technologies.” This
technology facilitates the remote exchange of reliable information for
diagnosis, treatment, and disease prevention [5].
The emergence of telemedicine, which leverages
telecommunication technologies to deliver and support remote healthcare, has
ushered in a new era in healthcare provision. It offers numerous opportunities
for improving patient outcomes and expanding access to medical care. Its
applications include real-time video consultations, remote monitoring, and
mobile health applications, all designed to bridge the gap between patients and
healthcare providers. Telemedicine’s potential for enhancing patient outcomes
and healthcare access is multifaceted, addressing longstanding challenges such
as geographical barriers, provider shortages, and the need for timely medical
interventions. Additionally, it eliminates the necessity for long-distance
travel for patients in rural or underserved areas, reducing both the time and
costs associated with accessing healthcare. Furthermore, it provides a platform
for continuous monitoring and follow-up care, which is essential for managing
chronic diseases and improving overall health outcomes. The convenience and
flexibility of telemedicine also contribute to increased patient engagement and
adherence to treatment plans [6].
Telemedicine-based solutions are among the most effective
approaches for improving patient care quality and promoting self-management in patients
[7, 8]. According to the WHO,
“self-care” is defined as the ability of individuals, families, and communities
to promote health, prevent disease, maintain well-being, and cope with illness
and disability, with or without the support of a healthcare provider [9]. Access to technologies such as telemedicine enables
patients to take a more active role in their health-related activities, thereby
increasing their opportunities for self-care [10, 11].
In this regard, the widespread adoption of mobile
technology is being leveraged to enhance healthcare delivery. A broad range of
health applications has been introduced for monitoring, planning, and achieving
health-related goals. Given these advancements, smartphones have gradually
become an integral part of daily life, offering immense value in routine tasks.
Today, compared to the past, smartphones provide a wider array of functions and
features [12].
With the widespread use of smartphones and the expansion
of telemedicine, accessing medical services has become significantly easier.
Individuals can now conveniently obtain medical appointments, receive online
consultations, and manage their electronic health records [13].
As self-care and telemedicine gain traction among
patients, the number of e-health applications has increased exponentially in
recent years [14]. However, there is a growing body of
reports indicating that various usability deficiencies in these applications,
as well as in the environments where they are deployed, may ultimately affect
the quality of patient care [15].
Among the various factors
contributing to the abandonment or failure of an application, poor usability
remains one of the most critical barriers to its widespread adoption [16-18].
Usability refers to the ease with which users can learn,
interact with, and efficiently use a system, encompassing factors such as
learnability, efficiency, memorability, error prevention, and user
satisfaction. Therefore, evaluating the usability of health information systems
is essential for ensuring their effectiveness and user adoption [19-23].
A crucial component of self-care is the ability of
individuals to actively participate in their health management through healthy
lifestyle choices [24]. Studies suggest that 60% of
diseases can be prevented through effective self-care [25].
Chronic diseases pose a significant challenge to
healthcare systems, and self-care behaviors play a crucial role in managing and
treating chronic conditions [26]. Research has shown that
when patients have access to health technologies that empower them to take an
active role in their healthcare, their engagement in self-care significantly
improves [27].
Over the past few centuries, the sharing of medical
knowledge and telemedicine have evolved through technological advancements,
including the printing press, telegraph, telephone, and the internet [28].
Today, mobile technologies are more accessible than ever
and have been widely adopted in both the public and private sectors. One of the
most promising applications of mobile technology is its role in health
monitoring and management. Mobile health (mHealth) refers to any health-related
service that utilizes mobile devices, including phones, tablets, and wireless
technologies [29].
Through mobile health technologies, patients can monitor
their treatments, manage health-related concerns, and receive timely medical
assistance. These technologies are rapidly evolving, transforming how
healthcare services are delivered and accessed worldwide [30-32].
While smartphone applications have the potential to
enhance healthcare quality and accessibility, studies have identified usability
challenges that hinder effective user interaction with these applications.
Issues such as poor user-centered design, privacy concerns, and lack of
reliability in emergency situations have been cited as barriers to adoption [33].
The International Organization for Standardization (ISO)
defines usability as “the extent to which a product can be used by specified
users to achieve specified goals with effectiveness, efficiency, and
satisfaction in a specified context of use” [14].
As usability becomes a critical factor in the adoption of
digital health applications, ensuring that these technologies are well-designed
and tailored to the needs of end-users is essential. This requires robust
usability evaluation methodologies to guarantee a seamless user experience.
Conducting usability assessments for digital health
applications offers substantial benefits, including enhanced efficiency,
improved user well-being, reduced stress, increased accessibility, and a lower
risk of user errors [34].
Usability evaluations help identify and address design
flaws that may negatively impact user interaction with web applications and
digital health platforms [35]. A well-designed health
information system with high usability can significantly improve healthcare
delivery, reduce errors, increase efficiency, and enhance user satisfaction [36]. Previous studies have demonstrated that usability
issues—such as unclear system messages and inefficient workflows—can reduce
user efficiency and hinder successful system interactions [37].
Various usability evaluation methods exist, depending on
factors such as the design phase, system complexity, target users, budget, and
time constraints [38, 39].
Material and Methods
Participants
The participants in this study were categorized into
three groups: users, facilitators, and technical support staff. The user group
consisted of 15 health information technology students from Varastegan
Institute for Medical Sciences. These individuals possessed knowledge of mobile
health application design, analysis, and user interface principles, but had no
prior experience with the Doctor Saina application. These users could
potentially serve as future system users. This study was conducted in
compliance with the ethical standards outlined in the Helsinki Declaration.
Before the evaluation commenced, participants were briefed on the study’s
objectives and general framework. Written and verbal informed consent was
obtained from all participants. Furthermore, their personal information was
handled confidentially, ensuring anonymity. Each user was accompanied by
a facilitator, who did not interfere with the evaluation process. Facilitators
only intervened if users encountered difficulties during usability testing,
reminding them to verbalize their thoughts. These facilitators were health
information technology specialists with experience in usability assessment. To
address potential technical issues during the evaluation, a software specialist
was also present as technical support.
Evaluation Tool
The evaluation was conducted in a quiet environment with
adequate lighting, a table, two chairs, and an Android smartphone with internet
access. Various tools were utilized to record user interactions, including:
•
Vidma REC (ver 2.6.14) to capture user interactions
with the application and verbal feedback.
•
A microphone and a video camera to record
participants’ voices and facial expressions.
A 15-part scenario comprising 10 usability tasks was
developed based on the application’s features (Appendix 1).
These tasks included:
1. User registration and profile editing
2. Accessing online medical consultations
3. Diagnosing conditions using the symptom checker
4. Assessing health status through the health checker
5. Reviewing the app’s health magazine
6. Exploring the at-home laboratory services
7. Accessing mental health services
8. Interacting with the health bank section
A widely accepted usability evaluation approach involves
real-user testing. In this study, the Think-Aloud method was employed, which is
an empirical approach focusing on observing users as they interact with the
system in real-time. This method gathers cognitive interaction data by
requiring participants to verbalize their observations, thoughts, emotions, and
decision-making processes while using the system.
Before the evaluation began, users received a 10-minute
training session on the Think-Aloud method, where they were instructed on how
to articulate their thoughts, emotions, and decisions in detail. After
completing the evaluation, participants were asked to provide suggestions for
improving the Doctor Saina application, which were documented in a structured
report form.
Analysis of Results
Following the completion of the assessments, the
researcher analyzed the recorded interactions, including Vidma REC files, audio
recordings, and user feedback reports. An independent review was conducted to
compile a comprehensive list of usability issues, along with their severity
levels.
Any discrepancies among researchers were resolved by
reviewing the recorded data.
For categorizing usability issues, the classification
method proposed by Van den Haak et al. was employed. According to this
approach, issues were grouped into four main categories:
•
Layout-related issues
•
Terminology-related issues
•
Data entry issues
•
Comprehensiveness issues
Apart from these four categories, users occasionally
encountered technological constraints, such as network connectivity problems.
Since these were not usability-related issues, they were excluded from the
analysis.
To assess the severity of usability problems, Nielsen’s
Heuristic Evaluation method was applied.
The Nielsen Questionnaire, developed by Jakob Nielsen,
includes ten fundamental principles for evaluating application usability:
1. System status visibility (awareness of navigation and
transitions);
2. Match between the system and the real world (use of familiar
terminology);
3. User control and freedom (easy navigation and exit options);
4. Consistency and adherence to standards;
5. Error prevention (minimization of incorrect data entry);
6. Recognition rather than recall;
7. Flexibility and efficiency of use;
8. Help users recognize, diagnose, and recover from errors;
9. Aesthetic and minimalist design;
10. Help
and documentation.
Using this heuristic framework, usability issues were
identified, and their potential impact on the user experience was assessed.
This method is widely recognized as an effective and cost-efficient approach
for evaluating clinical information systems and is extensively utilized in
usability assessments of user interfaces. According to Nielsen’s
classification, the severity of usability issues was categorized into five
levels (Table 1). However, issues ranked with a severity level of “0” were
excluded from the final list based on consensus among the researchers. Data
analysis was performed using SPSS (ver 26).
Table 1: Severity classification of usability
problems
|
Description
|
Severity
|
|
No usability problem
|
0
|
|
Cosmetic problem
|
1
|
|
Minor usability problem
|
2
|
|
Major usability problem
|
3
|
|
Usability catastrophe
|
4
|
Results
The user group in this study consisted of 15
participants, including 3 males (20%) and 12 females (80%), with an average age
of 20 years. The mean duration of the evaluation process for users was 22.08
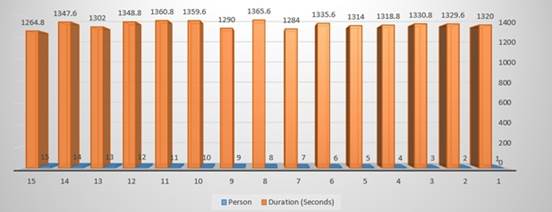
minutes. The evaluation time for each user is illustrated in Fig 1.
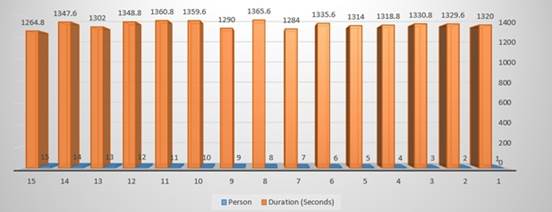
Fig 1: The evaluation time for each user
A total of 23 usability issues were identified by users
during the evaluation process. The categorization and severity levels of these
issues are presented in Table 2.
Among the identified issues, those related to
comprehensiveness were the most frequent, accounting for 10 cases (43.5%). As
shown in Table 2, approximately 40% of the issues in this category were
classified as minor (severity level 2).
The most frequently reported issue in this category was
the inability to enter miscellaneous symptoms in the disease diagnosis section
(Task 4), which was highlighted by 10 users. This was followed by the lack of
coordination for consultation regarding laboratory tests (Task 8), reported by
9 users.
As indicated in Table 2, layout-related issues accounted
for 4 cases (30.4%). Among these, 2 issues were rated as severity level 4. The
most frequently reported problems in this category were the absence of a
confirmation message after data entry (Task 3), reported by 10 users, and the
lack of proper categorization for physicians, reported by 8 users.
Table 2: Classification and Severity of
Usability Issues Identified by Users
|
Comprehensiveness
N (%)
|
Data entry
N (%)
|
Terminology
N (%)
|
Layout
N (%)
|
Variables
|
|
10(43.5)
|
3(13.0)
|
3(13.0)
|
7(30.4)
|
Usability Problem
|
|
5(50.0)
|
2(66.7)
|
2(66.7)
|
4(57.1)
|
1
|
Severity
|
|
4(40.0)
|
0
|
0
|
1(14.3)
|
2
|
|
1(10.0)
|
1(33.3)
|
0
|
0
|
3
|
|
0
|
0
|
1(33.3)
|
2(28.6)
|
4
|
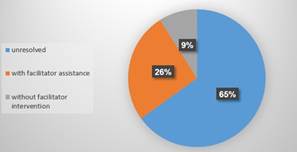
Fig 2 illustrates how usability issues were addressed by
users during the evaluation process.
According to this figure:
•
2 issues (9%) were resolved by users independently,
without facilitator intervention.
•
6 issues (26.0%) were resolved with facilitator
assistance, without interrupting the evaluation process.
•
15 issues (65.2%) remained unresolved after user
attempts and were bypassed, allowing the evaluation process to continue without
completing the associated tasks.
A summary of all identified issues by users and
specialists is presented in Table 3.
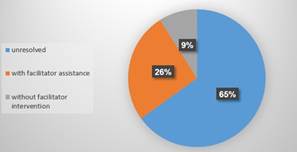
Fig 2: Illustrates how usability issues were
addressed by users during the evaluation process
During the 15 evaluations using the think-aloud method,
23 issues were identified, none of the users utilized the system’s help
feature. Additionally, 8 users provided suggestions for improving the system’s
performance. The most common suggestions were related to improving the design
of the doctor classification section and enhancing the notifications for
operations within the application’s service sections.
discussion
Usability studies of the Doctor Saina application in the
healthcare domain require serious attention. Usability is a crucial part of
developing this application, especially when the goal is to improve the
physical health of the patient. In this study, the usability of the Doctor
Saina application was evaluated using the think-aloud method. During the
evaluation process, 23 issues were identified by the users, 5 of which had a
severity greater than 2. While the participants generally assessed the
usability of the application as good, some issues remained that could be
addressed to improve the user experience. The most frequent usability issues
identified by users were in the Comprehensiveness category (43.5%). The two
most common issues were: the inability to record symptoms other than those
listed in the disease diagnosis section and the lack of a time frame for
scheduling phone consultations after a test request was made. These issues may
have arisen due to the limited options available in the symptom list, which may
not be comprehensive or aligned with user needs, and the lack of clarity in
scheduling physician availability.
During the evaluation process, 9% of the issues were
resolved by users without facilitator intervention. Additionally, 65% of the
issues remained unresolved, and 26% of the remaining issues were resolved with
the facilitator’s help.
Table 3: Identified Usability Issues
|
Issues
|
Users
|
|
Layout
|
1- The diagnostic tool lacks a
symptom search feature. (5 users / Severity: 4)
2- The psychological assessment
section does not include a back-navigation option. (6 users / Severity: 1)
3- Healthcare facility locations
are not integrated with navigation applications. (3 users / Severity: 1)
4- After completing registration
and updating their profile, users do not receive a confirmation message
(e.g., “Registration Successful”). (10 users / Severity: 1)
5- The specialty selection menu
for choosing a physician for medical consultation would be more user-friendly
if presented as a dropdown menu. (8 users / Severity: 4)
6- The active/inactive status of
physicians is not clearly visible to users. (3 users / Severity: 2)
7- The health database and
medical journal sections primarily contain text-based information, lacking
engaging graphical content. (3 users / Severity: 1)
|
|
Data entry
|
1- When applying filters to find
physicians, the results do not accurately reflect the selected filters. (7
users / Severity: 3)
2- Comments and reviews are not
restricted to patients who have had a consultation—any user, even without a
prior visit, can submit a review. (1 user / Severity: 1)
3- The validation process for
user profile data is not sufficiently robust. (2 users / Severity: 1)
|
|
Terminology
|
1- Instead of displaying an error
message when accessing the herbal medicine section, the system should provide
a message indicating the activation date. (15 users / Severity: 4)
2- The meaning of an “active” or
“inactive” physician was unclear to users. (4 users / Severity: 1)
3- The medical conditions
section within the health database is overly technical and not suitable for
general users. (2 users / Severity: 1)
|
|
Comprehensiveness
|
1-The physician recommendation
system is solely based on response time and frequency, without considering
physician experience or patient satisfaction. (1 user / Severity: 1)
2-The diagnostic tool lacks high
accuracy in identifying diseases. (8 users / Severity: 3)
3-Users cannot input symptoms
that are not already listed in the diagnostic section. (12 users / Severity:
1)
4-The recommended physician at
the end of the diagnosis process does not necessarily match the probable
diagnosis. (6 users / Severity: 2)
5-The search and filter
functions in the health database allow searches only by location, not by
medical specialty or condition. (3 users / Severity: 1)
6-Information regarding
healthcare service centers within the health database is not fully accurate.
(1 user / Severity: 1)
7-The reliability of
psychological assessments and their sources is not clearly stated. (2 users /
Severity: 2)
8-The application does not
include a section for submitting and tracking laboratory test requests. (1
user / Severity: 1)
9-No time frame is provided for
scheduling a follow-up call after requesting an at-home lab test. (9 users /
Severity: 2)
10-The integration of medical
consultation payments with insurance is problematic due to limited agreements
with different insurance providers. (7 users / Severity: 2)
|
The goal of usability testing is to identify usability
problems in the system and provide solutions for addressing these issues. In
this context, users made several suggestions to improve the system’s
performance. Most of these suggestions focused on improving the design and
categorization of certain fields, such as creating a more user-friendly
classification of doctors in the online medical consultation section.
One critical aspect that requires further review and
attention is for users who may face equipment limitations. It is recommended
that telephone-based support be provided for these users. Another consideration
is for users with visual, auditory, or physical impairments, for whom the
application’s features do not currently provide solutions. In the future,
solutions such as voice guidance, vibration, or non-verbal solutions could help
address these limitations.
One limitation of this study was that the evaluation
sessions were conducted in a laboratory setting. Users might interact with the
application more comfortably in a real-world environment, possibly having
different opinions on the issues and their severity. On the other hand, one of
the key strengths of this study was the precise think-aloud usability test of
the Doctor Saina online medical consultation application. Moreover, this study
is one of the few conducted in this area in Iran.
Question 1: What is the severity of issues related to
receiving online medical consultations in video, phone, and text formats?
This service is accessible in the “My Health” section of
the Doctor Saina application under the medical consultation section. The most
frequent usability issues encountered by users in online medical consultations
were in the Layout category. Two of the most common issues were related to the
categorization of doctors in the initial online medical consultation section.
It might be more effective to align the doctor categorization with the system
used for selecting treatment centers in the Health Bank section to allow for
easier specialization-based doctor selection.
Question 2: What is the severity of issues related to
receiving online laboratory services?
Access to this service is available in the “Tests at
Home” section of the Doctor Saina application. The most significant issue in
this section was related to Comprehensiveness. The user reported that after
submitting a test request, there was no time frame provided for coordination.
The application only stated that the user would be contacted “as soon as
possible,” but the user was not informed about the time range for the call.
Another issue was related to the inability of the user to use their supplemental
insurance due to the lack of an agreement between the application and the
user’s insurance company. This issue arose from the limitations in contracts
with different insurance companies. Since users prefer to use their
supplementary insurance over the free-market prices, this is a significant
factor.
Question 3: What is the severity of issues related to
receiving health and disease diagnosis services online?
Access to this service is available through the “My
Health” section of the Doctor Saina application. The most significant usability
issues in the health and disease diagnosis section were also in the
Comprehensiveness category. The first issue was related to the search and
selection of disease symptoms, where users could not find their symptoms in the
available list. Another issue was the inaccuracy of disease diagnosis based on
the symptoms entered by the users. Lastly, there was a mismatch between the doctor
and the disease according to the symptoms entered. This may have been caused by
inadequate categorization of the symptom, diagnosis, and specialty information.
Question 4: What is the severity of issues related to
receiving general information from the Health Magazine?
This section of the application is accessible through the
Health Magazine section. This section had the fewest issues for users, with the
only complaint being related to the lack of visual appeal and graphics, which
is a Layout issue.
Question 5: What is the severity of usability issues in
the Doctor Saina web application?
Users reported several significant issues with the Doctor
Saina application. One issue was the limitation of the symptom list in the
disease diagnosis section, which prevented users from entering symptoms outside
the predefined list. Additionally, most users experienced issues with not
receiving confirmation after editing and saving their profile information,
which was ranked with a severity of 1. Other common issues included the
inability to cooperate with different insurance companies and inaccuracies in
disease diagnosis, which were ranked with a severity of 2. The most frequent
issue related to the lack of access and awareness of the time for resuming
access to the pharmacy and herbal medicine sections of the Health Bank, as well
as the lack of proper categorization of specialties in the online medical consultation
section, both of which were identified as critical issues with a severity of 4.
If, after this study, the application management and
support team address these issues, it can enhance the accuracy of disease
diagnosis for users. Furthermore, if the application collaborates with various
insurance companies, users would no longer have to chase insurance claims after
consultations. Additionally, reducing the time users spend navigating the
application would lead to a more efficient and user-friendly experience.
Conclusion
The user evaluation of the Doctor Saina application
revealed that despite being a new application designed with attention to user
needs and established standards, several usability issues remain. The most
frequent issues were identified in the Comprehensiveness category. If these
problems are not addressed, they may negatively impact user performance,
leading to fatigue, confusion, wasted time, and, ultimately, user
dissatisfaction. This dissatisfaction could escalate into errors, reduced
treatment quality, and potentially jeopardize patient health.
The findings underscore the importance of adhering to
established human-computer interaction standards to prevent such issues.
Addressing the 23 identified usability issues and making the necessary
improvements will enhance the overall user experience. The management team of
the Doctor Saina web application has been notified of these issues, with
recommendations for improvement to ensure a more efficient and user-friendly
system.
Acknowledgement
This study was supported by Varastegan Institute for
Medical Sciences. We thank all participants for the collaboration in this
study.
Author’s contribution
FR:
Data acquisition, analysis, and interpretation of data, drafting the work; FM:
Acquisition, analysis, and interpretation of data, drafting the work; ZS:
Drafting the work, revising it critically for important intellectual content; HMR:
Drafting the work, revising it critically for important intellectual content; MRMH:
Design of the work, revising it critically for important intellectual content.
All authors contributed to the literature review, design,
data collection, drafting the manuscript, read and approved the final
manuscript.
Conflicts of interest
The authors declare no conflicts of interest regarding
the publication of this study.
Ethical Approval
This study was approved by the ethical committee of
Mashhad University of Medical Sciences (approval number IR.MUMS.REC.1402.034).
Financial disclosure
No financial interests related to the material of this
manuscript have been declared.
References
1.
Dorsey ER, Topol EJ. State of telehealth. N Engl J
Med. 2016; 375(2): 154-61. PMID: 27410924 DOI: 10.1056/NEJMra1601705
[PubMed]
2.
Parikh D, Armstrong G, Liou V, Husain D. Advances
in telemedicine in ophthalmology. Semin Ophthalmol. 2020; 35(4): 210-5. PMID: 32644878 DOI: 10.1080/08820538.2020.1789675 [PubMed]
3.
Hadziahmetovic M, Nicholas P, Jindal S, Mettu PS,
Cousins SW. Evaluation of a remote diagnosis imaging model vs dilated eye
examination in referable macular degeneration. JAMA Ophthalmol. 2019; 137(7): 802-8.
PMID: 31095245 DOI: 10.1001/jamaophthalmol.2019.1203 [PubMed]
4.
Su Z, Li C, Fu H, Wang L, Wu M, Feng X. Development
and prospect of telemedicine. Intelligent Medicine. 2024; 4(1): 1-9.
5.
Naik N, Ibrahim S, Sircar S, Patil V, Hameed BM,
Rai BP, et al. Attitudes and perceptions of outpatients towards adoption of
telemedicine in healthcare during COVID-19 pandemic. Ir J Med Sci. 2022; 191(4):
1505-12. PMID: 34402031 DOI: 10.1007/s11845-021-02729-6
[PubMed]
6.
Ezeamii VC, Okobi OE, Wambai-Sani H, Perera GS,
Zaynieva S, Okonkwo CC, et al. Revolutionizing healthcare: How telemedicine is
improving patient outcomes and expanding access to care. Cureus. 2024; 16(7): e63881.
PMID: 39099901 DOI: 10.7759/cureus.63881 [PubMed]
7.
Gholamzadeh M, Abtahi H, Safdari R. Telemedicine in
lung transplant to improve patient-centered care: A systematic review. Int J
Med Inform. 2022; 167: 104861. PMID: 36067628 DOI: 10.1016/j.ijmedinf.2022.104861
[PubMed]
8.
Aalaei S, Amini M, Mazaheri Habibi MR, Shahraki H,
Eslami S. A telemonitoring system to support CPAP therapy in patients with
obstructive sleep apnea: A participatory approach in analysis, design, and
evaluation. BMC Med Inform Decis Mak. 2022; 22(1): 168. PMID:
35754055 DOI: 10.1186/s12911-022-01912-8
[PubMed]
9.
World Health Organization. Diabetes [Internet].
2024 [cited: 25 Sep 2024]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/diabetes
10.
Agarwal E, Miller M, Yaxley A, Isenring E.
Malnutrition in the elderly: A narrative review. Maturitas. 2013; 76(4): 296-302.
PMID: 23958435 DOI: 10.1016/j.maturitas.2013.07.013 [PubMed]
11.
Agha Seyyed Esmaeil Amiri FS, Bohlouly F,
Khoshkangin A, Razmi N, Ghaddaripouri K, Mazaheri Habibi MR. The effect of
telemedicine and social media on cancer patients' self-care: A systematic
review. Frontiers in Health Informatics. 2021; 10: 92.
12.
Mubeen M, Iqbal MW, Junaid M, Sajjad MH, Naqvi MR,
Khan BA, et al. Usability evaluation of pandemic health care mobile
applications. IOP conference series: Earth and environmental science; 2021.
13.
Al-Marsy A, Chaudhary P, Rodger JA. A model for
examining challenges and opportunities in use of cloud computing for health
information systems. Applied System Innovation. 2021; 4(1): 15.
14.
Maramba I, Chatterjee A, Newman C. Methods of
usability testing in the development of eHealth applications: A scoping review.
Int J Med Inform. 2019; 126: 95-104. PMID: 31029270 DOI: 10.1016/j.ijmedinf.2019.03.018
[PubMed]
15.
Watbled L, Marcilly R, Guerlinger S, Bastien JM,
Beuscart-Zéphir MC, Beuscart R. Combining usability evaluations to highlight
the chain that leads from usability flaws to usage problems and then negative
outcomes. J Biomed Inform. 2018; 78: 12-23. PMID: 29305953 DOI: 10.1016/j.jbi.2017.12.014
[PubMed]
16.
Khajouei R, Hasman A, Jaspers MW. Determination of
the effectiveness of two methods for usability evaluation using a CPOE
medication ordering system. Int J Med Inform. 2011; 80(5): 341-50. PMID: 21435943 DOI: 10.1016/j.ijmedinf.2011.02.005 [PubMed]
17.
Campbell EM, Guappone KP, Sittig DF, Dykstra RH,
Ash JS. Computerized provider order entry adoption: Implications for clinical
workflow. J Gen Intern Med. 2009; 24(1): 21-6. PMID: 19020942 DOI: 10.1007/s11606-008-0857-9
[PubMed]
18.
Kim MS, Shapiro JS, Genes N, Aguilar MV, Mohrer D,
Baumlin K, et al. A pilot study on usability analysis of emergency department
information system by nurses. Appl Clin Inform. 2012; 3(1): 135-53. PMID: 23616905 DOI: 10.4338/ACI-2011-11-RA-0065 [PubMed]
19.
Khajouei R, Azizi AA, Atashi A. Usability
evaluation of an emergency information system: A heuristic evaluation. Journal
of Health Administration. 2013; 16(52): 61-72.
20.
Nielsen J. Usability engineering. Academic Press;
1993.
21.
Mazaheri Habibi MR, Khajouei R, Eslami S, Jangi M,
Ghalibaf AK, Zangouei S. Usability testing of bed information management
system: A think-aloud method. J Adv Pharm Technol Res. 2018; 9(4): 153-7. PMID: 30637234 DOI: 10.4103/japtr.JAPTR_320_18 [PubMed]
22.
Ghalibaf AK, Jangi M, Mazaheri Habibi MR, Zangouei
S, Khajouei R. Usability evaluation of obstetrics and gynecology information
system using cognitive walkthrough method. Electron Physician. 2018; 10(4): 6682-8.
PMID: 29881531 DOI: 10.19082/6682 [PubMed]
23.
Jangi M, Khajouei R, Tara M, Mazaheri Habibi MR,
Ghalibaf AK, Zangouei S, et al. User testing of an admission, discharge,
transfer system: Usability evaluation. Frontiers in Health Informatics. 2021; 10:
77.
24.
Narasimhan M, Kapila M. Implications of self-care
for health service provision. Bull World Health Organ. 2019; 97(2): 76-A. PMID: 30728611 DOI: 10.2471/BLT.18.228890 [PubMed]
25.
Zhang X, Foo S, Majid S, Chang Y-K, Dumaual HTJ,
Suri VR. Self-care and health-information-seeking behaviours of diabetic
patients in Singapore. Health Commun. 2020; 35(8): 994-1003. PMID: 31303050 DOI: 10.1080/10410236.2019.1606134 [PubMed]
26.
Koirala B, Himmelfarb CRD, Budhathoki C, Davidson
PM. Heart failure self-care, factors influencing self-care and the relationship
with health-related quality of life: A cross-sectional observational study. Heliyon.
2020; 6(2): e03412. PMID: 32149197 DOI: 10.1016/j.heliyon.2020.e03412 [PubMed]
27.
Jin MX, Kim SY, Miller LJ, Behari G, Correa R.
Telemedicine: Current impact on the future. Cureus. 2020; 12(8): e9891. PMID: 32968557 DOI: 10.7759/cureus.9891 [PubMed]
28.
Seppälä J, De Vita I, Jämsä T, Miettunen J,
Isohanni M, Rubinstein K, et al. Mobile phone and wearable sensor-based mHealth
approaches for psychiatric disorders and symptoms: Systematic review. JMIR Ment
Health. 2019; 6(2): e9819. PMID: 30785404 DOI: 10.2196/mental.9819
[PubMed]
29.
Tas B, Lawn W, Traykova EV, Evans RA, Murvai B,
Walker H, et al. A scoping review of mHealth technologies for opioid overdose
prevention, detection and response. Drug Alcohol Rev. 2023; 42(4): 748-64. PMID: 36933892 DOI: 10.1111/dar.13645 [PubMed]
30.
Torous J, Nicholas J, Larsen ME, Firth J,
Christensen H. Clinical review of user engagement with mental health smartphone
apps: Evidence, theory and improvements. Evid Based Ment Health. 2018; 21(3): 116-9.
PMID: 29871870 DOI: 10.1136/eb-2018-102891 [PubMed]
31.
Moghbeli F, Setoodefar M, Mazaheri Habibi MR,
Abbaszadeh Z, Keikhay Moghadam H, Salari S, et al. Using mobile health in
primiparous women: Effect on awareness, attitude and choice of delivery type,
semi-experimental. Reprod Health. 2024; 21(1): 49. PMID: 38594731 DOI: 10.1186/s12978-024-01785-2
[PubMed]
32.
Khoshkangin A, Agha Seyyed Esmaeil Amiri FS,
Ghaddaripouri K, Noroozi N, Mazaheri Habibi MR. Investigating the role of
mobile health in epilepsy management: A systematic review. J Educ Health
Promot. 2023; 12: 304. PMID: 38023071 DOI: 10.4103/jehp.jehp_1188_22
[PubMed]
33.
Agapito G, Cannataro M. An overview on the challenges
and limitations using cloud computing in healthcare corporations. Big Data and
Cognitive Computing. 2023; 7(2): 68.
34.
Greenhalgh T, Wherton J, Papoutsi C, Lynch J,
Hughes G, Hinder S, et al. Beyond adoption: A new framework for theorizing and
evaluating nonadoption, abandonment, and challenges to the scale-up, spread,
and sustainability of health and care technologies. J Med Internet Res. 2017; 19(11):
e367. PMID: 29092808 DOI: 10.2196/jmir.8775 [PubMed]
35.
Lawal FB, Omara M. Applicability of dental patient
reported outcomes in low resource settings–a call to bridge the gap in clinical
and community dentistry. J Evid Based Dent Pract. 2023; 23(1S): 101789. PMID: 36707169 DOI: 10.1016/j.jebdp.2022.101789 [PubMed]
36.
Oliveira Chaves L, Gomes Domingos AL, Louzada
Fernandes D, Ribeiro Cerqueira F, Siqueira-Batista R, Bressan J. Applicability
of machine learning techniques in food intake assessment: A systematic review. Crit
Rev Food Sci Nutr. 2023; 63(7): 902-19. PMID: 34323627 DOI: 10.1080/10408398.2021.1956425
[PubMed]
37.
Damiani M, Sinkko T, Caldeira C, Tosches D,
Robuchon M, Sala S. Critical review of methods and models for biodiversity
impact assessment and their applicability in the LCA context. Environmental
Impact Assessment Review. 2023; 101: 107134.
38.
Thyvalikakath TP, Monaco V, Thambuganipalle H,
Schleyer T. Comparative study of heuristic evaluation and usability testing
methods. Stud Health Technol Inform. 2009; 143: 322-7. PMID: 19380955 [PubMed]
39.
Yen PY, Bakken S. A comparison of usability
evaluation methods: Heuristic evaluation versus end-user think-aloud protocol –
An example from a web-based communication tool for nurse scheduling. AMIA Annu
Symp Proc. 2009; 2009: 714-8. PMID: 20351946 [PubMed]
Appendices
Appendix 1
1. Usability Evaluation Scenario of the Doctor Saina Application
2. In the first task, the user must open the application and
register as a user by providing their personal information.
3. In the second task, the user accesses their profile section and
completes or edits their personal information.
4. Additionally, in the profile section, the user encounters
several items related to their user profile, which we asked them to review.
These items include: My Conversations, My Doctors, My Appointments, Favorites,
Financial Transactions, Support Requests, Frequently Asked Questions, Referral
to Friends, and Rating Doctor Saina.
5. In the third task, the user proceeds to the “My Health” section
to initiate an online medical consultation.
6. In this section, based on the user’s selection of a specialty or
doctor, they can choose to receive a consultation either by phone, urgent phone
call, text, or video, according to various criteria such as user reviews, the
doctor’s medical background, and successful consultations.
7. If the selected doctor is available, the user proceeds with the
consultation by choosing their primary and supplementary insurance and making
the payment.
8. If the doctor is unavailable, the user can either select an
alternative doctor or be notified when their chosen doctor becomes available.
9. In the fourth task, the user must use the “Disease
Diagnostician” section within the “My Health” section to begin the diagnostic
process for a potential illness based on their symptoms.
10. After
completing the diagnostic steps, the possible diagnosis is presented, and the
user can schedule a consultation with a doctor for further confirmation if
necessary.
11. In
the fifth task, the user is required to complete information in the “My Health”
section to receive a body health analysis.
12. In
the sixth task, the user must check useful and categorized health-related
articles in the “Health Magazines” section of Doctor Saina’s services.
13. In
the seventh task, the user can view their medical consultation history in the
“Conversations” section, categorized as: All, Pending Payment, and Completed.
14. In
the eighth task, the user can request an in-home laboratory test service
through the “Home Testing” section, and receive an interpretation of their test
results with the assistance of doctors.
15. In
the ninth task, the user can take a psychological test and receive analysis and
counseling in the “Psychological Testing” section.
16. In
the tenth task, the user can utilize the “Health Bank” section to access
information on medical centers, health services across the country, as well as
information on medications, herbal drugs, and diseases.